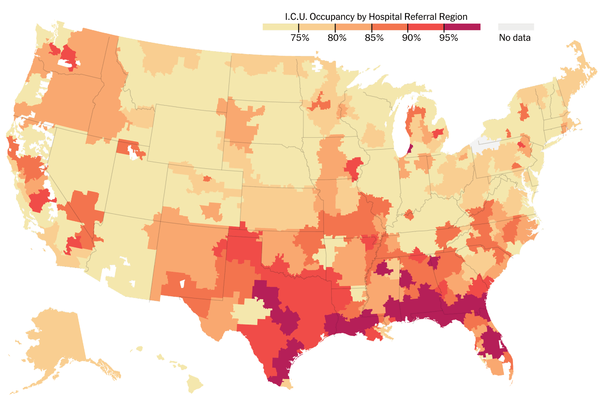
Covid-19 lays bare health disparities in black community
Author Profile
Latest entries
 Selected Media06/03/2025Canada to expedite nation building projects to counter Trump
Selected Media06/03/2025Canada to expedite nation building projects to counter Trump Economic Development06/03/2025Tulsa plans $105m in reparations for America’s ‘hidden’ massacre
Economic Development06/03/2025Tulsa plans $105m in reparations for America’s ‘hidden’ massacre Political Corruption05/29/2025The US military, eyeing China deterrence, could draw down deployments to South Korea
Political Corruption05/29/2025The US military, eyeing China deterrence, could draw down deployments to South Korea Political Corruption05/29/2025Federal court blocks Trump from imposing sweeping tariffs under emergency powers law
Political Corruption05/29/2025Federal court blocks Trump from imposing sweeping tariffs under emergency powers law